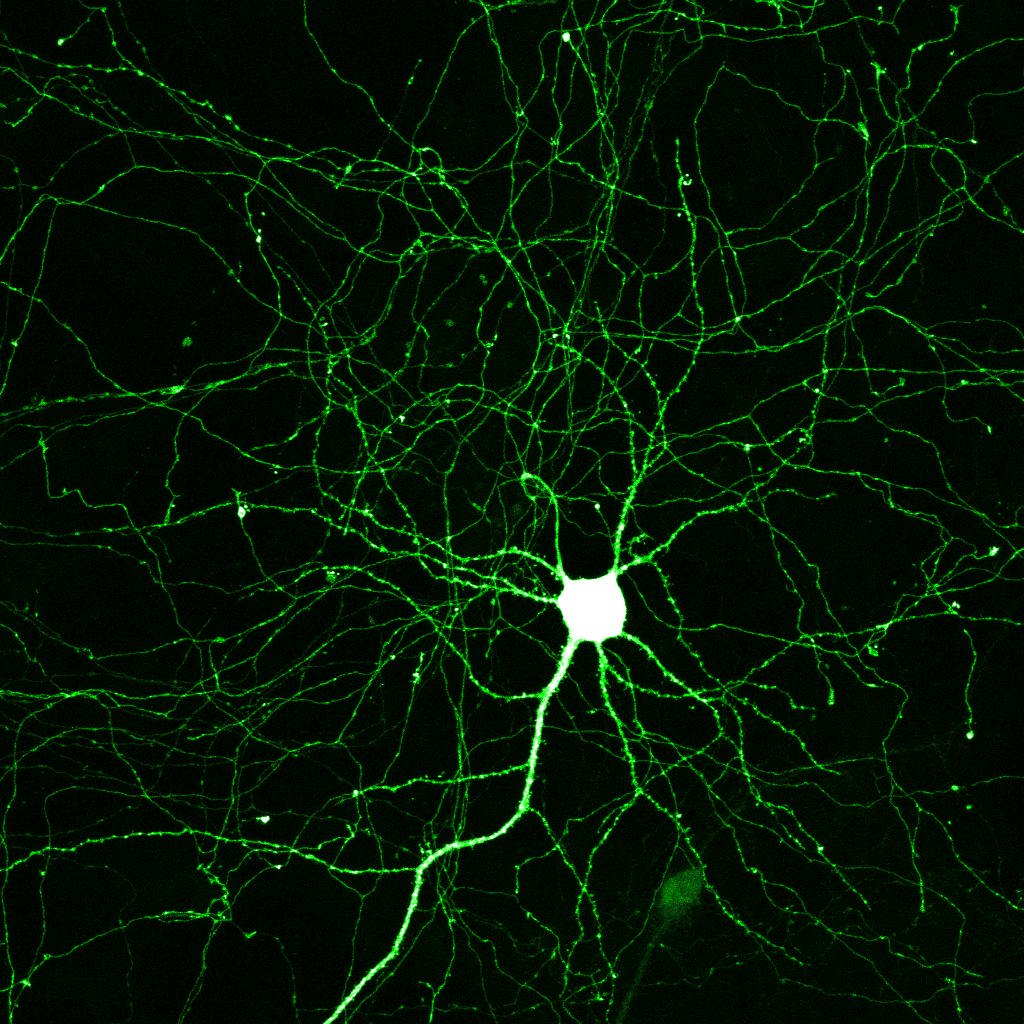
A neuron is an electrically excitable cell that processes and transmits information by electrochemical signaling, via connections with other cells called synapses. Neurons are the core components of nervous system, which includes the brain, spinal cord, and peripheral ganglia.
Transplanting fetal neurons into the brains of young mice opens a new window on neural plasticity, or flexibility in the brain’s neural circuits. The research, published today in the journal Science, suggests that the brain’s ability to radically adapt to new situations might not be permanently lost in youth, and helps to pinpoint the factors needed to reintroduce this plasticity.
A better understanding of brain plasticity could one day point to new ways to treat brain injury and other neurological problems by returning the brain to a younger, more malleable state. “[The findings] reveal there must be a factor that can induce plasticity in the brain,” says Michael Stryker, a neuroscientist at the University of California, San Francisco, who was involved in the research. “We hope that future studies will reveal what it is that allows the cells to induce this new period of plasticity.”
In the study, researchers examined a well-known phenomenon seen in the visual system of both mice and humans, during what is known as the “critical period” of development. If young animals are deprived of visual input in one eye during this stretch–about 25 to 30 days of age in mice–their visual systems will rewire to maximize visual input from the functioning eye. As a result, vision in the other eye is permanently impaired. “The cortex says, ‘I’m not getting information from this side, so just pay attention to other eye,’ ” says Arturo Alvarez-Buylla, also part of the UCSF team. After the critical period, depriving one eye of input has little long-term impact on vision.
To try to find out what triggers the neural plasticity seen during this period, the researchers took a specific type of neuron from the brains of fetal mice and grafted them into mice that had either just been born or were approximately 10 days old. Known as inhibitory interneurons, these cells release a chemical signal that quiets neighboring cells, making it more difficult for them to fire. The transplanted neurons, labeled with a fluorescent marker, began migrating to their normal place in the brain and making connections with resident neurons.
The mice went through the typical critical period, at about 28 days of age. But the transplanted neurons seemed to induce a second critical period, which was timed to the age of the transplanted cells rather than the age of the animals. The later critical period occurred when the transplanted neurons were about 33 to 35 days old, the same age as resident inhibitory interneurons during the normal critical period. (The neurons arise in the brain before birth.)
Scientists aren’t yet sure how the cells induce this second period of malleability. Stryker’s team and others had previously shown that the cells’ inhibitory signaling plays a key role–the critical period can be delayed or induced earlier by mimicking the inhibitory effects of the cells with drugs, such as valium. But in these previous experiments, it was not possible to induce a second critical period after the normal one. “Once you’ve had it, can never get another one, at least until these transplant experiments,” says Stryker. “That shows there is something other than just the inhibitory [chemical] they release that must be involved in this process.” Researchers plan to transplant different types of inhibitory neurons, in an attempt to find the specific cell type responsible.
“I would love to see if the same sort of transplant worked in older animals,” says Jianhua Cang, neuroscientist at Northwestern University, in Chicago. “This work is a significant advance, but if one can do it in adult animals, it would be even more remarkable. And it opens the possibility of therapeutic potential.” Cang was not involved in the current research, thought he has previously worked with the authors.
The findings could have wide-reaching implications for how we think about the nature of plasticity in the brain. Humans have a similar critical period, though in humans this phase is more extended than in mice. Infants and children with a lazy eye or a cataract will suffer permanent vision loss if the problem isn’t corrected before about eight years of age, says Takao Hensch, a neuroscientist at Children’s Hospital Boston, who was not involved in the current study. (During normal development, this period of plasticity is thought to be important for developing balanced input from both eyes, which is crucial for binocular vision.
The phenomenon isn’t limited to the visual system–scientists think that most parts of the cortex undergo a similar period of heightened malleability. For example, children fail to hear certain sounds after a particular age. “The classic example is kids growing up in Japan,” says Hensch. “They eventually lose the ability to differentiate between ‘R’ and ‘L’ sounds.”
If scientists can find a controlled way to trigger plasticity in specific parts of the brain, it would open new avenues for treatment of a variety of ailments. Adults who suffer brain damage from stroke or head trauma have some level of reorganization in the brain–enhancing that plasticity might improve recovery.
“Many psychiatric illnesses are recognized as having neurodevelopmental origins, in particular, deficits in inhibitory circuits,” says Hensch. For example, many genes linked to autism may trigger an imbalance in excitation and inhibition in neural signaling, he says. “If you can restore that imbalance, you might imagine intervening during development or later in life to try to restore brain function.”
Still, a long road lies ahead. To apply this type of cell transplant to humans, scientists would first need to develop a reliable source of the necessary cells, perhaps from induced pluripotent stem cell reprogramming. They would then need to show the cells can be safely transplanted into the brain. Figuring out how to properly capitalize on the newfound plasticity presents another hurdle. It’s not clear whether patients would need some kind of specific training or drug treatment to properly reorganize damaged neural circuits. “For higher cognitive functions, you might need to train people cognitively in the presence of plasticity-enhancing neurons,” says Hensch.
“Ideally, it would be nice to find a way to coax [the birth of new neurons in the brain] through some pharmacological or environmental means to get more of these inhibitory cells to appear,” he says. “That seems like quite a challenge, but this research gives us hope it’s worth trying.”